Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (27): 4265-4270.doi: 10.3969/j.issn.2095-4344.2014.27.001
Effect of recombinant human B-type natriuretic peptide on renal hemodynamics in a bioengineering model of acute myocardial infarction with heart failure
Fan Xin-na1, Zhang Jing2, Cai Li-li1, Yang Gui-feng1, Fu Xiang-hua3
- 1 Second Department of Geriatrics, the First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China; 2 CCU, the First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China; 3Second Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China
-
Online:2014-06-30Published:2014-06-30 -
Contact:Zhang Jing, M.D., Associate chief physician, CCU, the First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China -
About author:Fan Xin-na, Master, Attending physician, Second Department of Geriatrics, the First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China -
Supported by:the National Natural Science Foundation of China, No. 30871086; Medical Science Research Key Project of Hebei Province in 2011, No. 20110638
CLC Number:
Cite this article
Fan Xin-na, Zhang Jing, Cai Li-li, Yang Gui-feng, Fu Xiang-hua. Effect of recombinant human B-type natriuretic peptide on renal hemodynamics in a bioengineering model of acute myocardial infarction with heart failure[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(27): 4265-4270.
share this article
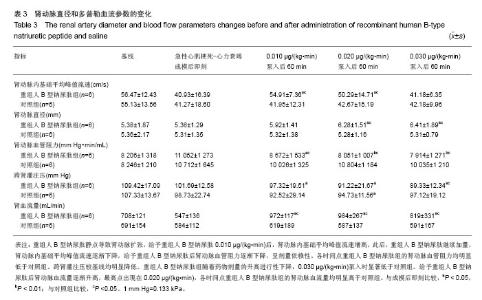
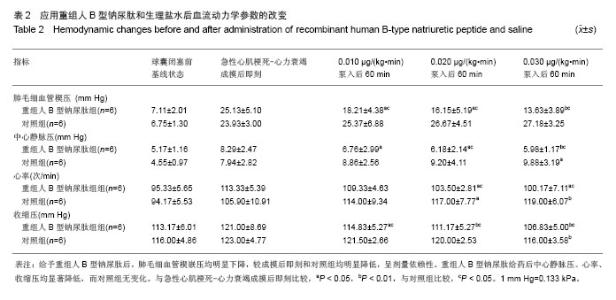
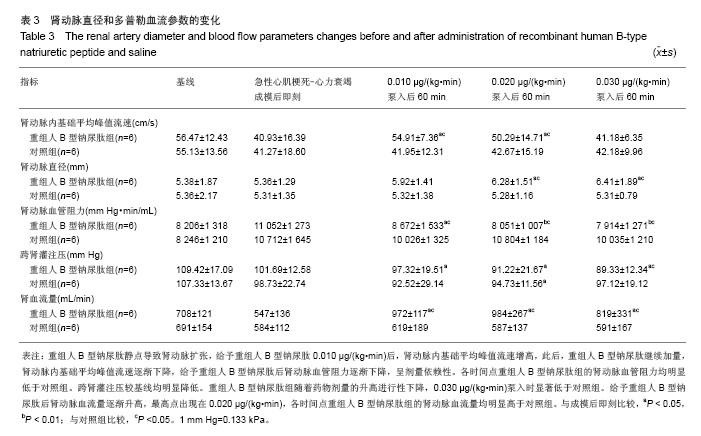
2.3 肾动脉直径、多普勒血流指标的变化 见表3。 血管造影显示,重组人B型钠尿肽静点导致肾动脉扩张,成模后管径和给予0.010,0.020和0.030 μg/(kg•min)泵入60 min时管径分别为(5.36±1.29) mm,(5.92±1.41) mm,(6.28±1.51) mm,(6.41±1.89) mm,差异有显著性意义。 成模后即刻,肾动脉内基础平均峰值流速较基线明显下降[(40.93±16.39) cm/s比(56.47±12.43) cm/s,P < 0.05],给予重组人B型钠尿肽0.010 μg/(kg•min)后,肾动脉内基础平均峰值流速增高,此后,重组人B型钠尿肽继续加量,肾动脉内基础平均峰值流速逐渐下降,0.03 μg/(kg•min)时最低为(41.18±6.35) cm/s。0.010 μg/(kg•min)泵入60 min和0.020 μg/(kg•min)泵入60 min时测定肾动脉内基础平均峰值流速,重组人B型钠尿肽组均明显高于对照组。 成模后肾动脉血管阻力较基线明显升高,而给予重组人B型钠尿肽后肾动脉血管阻力逐渐下降,呈剂量依赖性。各时间点重组人B型钠尿肽组的肾动脉血管阻力均明显低于对照组。 成模后即刻测定两组跨肾灌注压,较基线均明显降低。重组人B型钠尿肽组随着药物剂量的升高进行性下降,0.030 μg/(kg•min)泵入时显著低于对照组[(89.33± 12.34) mm Hg比(97.12±19.12) mm Hg,P < 0.05]。 成模后肾动脉血流量显著低于基线,给予重组人B型钠尿肽后肾动脉血流量逐渐升高,最高点出现在 0.020 μg/(kg•min),各时间点重组人B型钠尿肽组的肾动脉血流量均明显高于对照组。 "
| [1]重组人脑利钠肽多中心研究协作组.重组人脑利钠肽治疗心力衰竭安全性和疗效的开放性随机对照多中心临床研究[J].中华心血管病杂志,2011,39(4):305-308.
[2]O'Connor CM, Starling RC, Hernandez AF, et al.Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365(1):32-43.
[3]Elkayam U, Akhter MW, Singh H,et al.Comparison of effects on left ventricular filling pressure of intravenous nesiritide and high-dose nitroglycerin in patients with decompensated heart failure.Am J Cardiol. 2004;93(2):237-240.
[4]张晶,傅向华,贾辛未,等.重组人B型利钠肽治疗老年急性前壁心肌梗死合并收缩性心力衰竭患者的疗效和安全性[J].中国老年学杂志,2010,30(4):438-440.
[5]Charles CJ, Jardine DL, Rademaker MT,et al.Low dose B-type Natriuretic Peptide Raises Cardiac Sympathetic Nerve Activity in Sheep.Am J Physiol Regul Integr Comp Physiol. 2014. [Epub ahead of print]
[6]Hu G, Huang X, Zhang K,et al.Anti-inflammatory Effect of B-Type Natriuretic Peptide Postconditioning During Myocardial Ischemia-Reperfusion: Involvement of PI3K/Akt Signaling Pathway.Inflammation. 2014. [Epub ahead of print]
[7]Edvinsson ML, Uddman E, Edvinsson L,et al.Brain natriuretic peptide is a potent vasodilator in aged human microcirculation and shows a blunted response in heart failure patients.J Geriatr Cardiol. 2014;11(1):50-56.
[8]Demerath T, Staffel J, Schreiber A,et al.Natriuretic peptides buffer renin-dependent hypertension.Am J Physiol Renal Physiol. 2014. [Epub ahead of print]
[9]Wang S, Qu X, Qu Y,et al.The effect of B-type brain natriuretic peptide on patients with acute decompensated heart failure coexisting with lung cancer: a randomized controlled clinical trial.Pharmazie. 2014;69(3):212-216.
[10]Campbell KL, Johnson DW, Bauer JD,et al.A randomized trial of sodium-restriction on kidney function, fluid volume and adipokines in CKD patients.BMC Nephrol. 2014;15:57.
[11]Thireau J, Karam S, Roberge S,et al.β-Adrenergic blockade combined with subcutaneous B-type natriuretic peptide: a promising approach to reduce ventricular arrhythmia in heart failure?Heart. 2014;100(11):833-841.
[12]Sackner-Bernstein JD, Skopicki HA, Aaronson KD.Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure.Circulation. 2005;111 (12):1487-1491.
[13]Wu VC, Wu CH, Huang TM,et al.Long-term risk of coronary events after AKI.J Am Soc Nephrol. 2014;25(3):595-605.
[14]Cravedi P, Remuzzi G.Treating the kidney to cure the heart. Kidney Int Suppl. 2008;(111):S2-3.
[15]Zhang J, Fu X, Jia X,et al.B-type natriuretic peptide for prevention of contrast-induced nephropathy in patients with heart failure undergoing primary percutaneous coronary intervention.Acta Radiol. 2010;51(6):641-648.
[16]Arora S, Clarke K, Srinivasan V, et al.Effect of nesiritide on renal function in patients admitted for decompensated heart failure.QJM. 2007;100(11):699-706.
[17]Chen HH, Anstrom KJ, Givertz MM,et al.Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA. 2013;310(23):2533-2543.
[18]Spiliopoulos S, Guersoy D, Koerfer R,et al.B-type natriuretic peptide therapy in total artificial heart implantation: Renal effects with early initiation.J Heart Lung Transplant. 2014. [Epub ahead of print]
[19]Chow SL, Peng JT, Okamoto MP,et al.Effect of nesiritide infusion duration on renal function in acutely decompensated heart failure patients.Ann Pharmacother. 2007;41(4):556-561.
[20]Gottlieb SS, Stebbins A, Voors AA,et al.Effects of nesiritide and predictors of urine output in acute decompensated heart failure: results from ASCEND-HF (acute study of clinical effectiveness of nesiritide and decompensated heart failure).J Am Coll Cardiol. 2013;62(13):1177-1183.
[21]Elkayam U, Janmohamed M, Hatamizadeh P,et al.Impact of acute serum creatinine elevation in patients treated with nesiritide.Clin Cardiol. 2009;32(4):215-219.
[22]Witteles RM, Kao D, Christopherson D,et al.Impact of nesiritide on renal function in patients with acute decompensated heart failure and pre-existing renal dysfunction a randomized, double-blind, placebo-controlled clinical trial.J Am Coll Cardiol. 2007;50(19):1835-1840.
[23]Mentzer RM Jr, Oz MC, Sladen RN,et al.Effects of perioperative nesiritide in patients with left ventricular dysfunction undergoing cardiac surgery:the NAPA Trial.J Am Coll Cardiol. 2007;49(6):716-726.
[24]Hauptman PJ, Schnitzler MA, Swindle J,et al.Use of nesiritide before and after publications suggesting drug-related risks in patients with acute decompensated heart failure.JAMA. 2006; 296(15):1877-1884.
[25]张晶,傅向华,贾辛未,等.超选左前降支微血栓微球混悬液分次灌注构建小型猪急性心肌梗死后缺血性心力衰竭组织工程学模型[J].中国组织工程研究与临床康复,2010,14(20):3691-3695.
[26]张晶,傅向华,贾辛未,等. 小型猪急性心肌梗死后心力衰竭模型的构建[J]. 中国实验动物学报,2010,18(1):33-36.
[27]Burger AJ.A review of the renal and neurohormonal effects of B-type natriuretic peptide.Congest Heart Fail. 2005;11(1): 30-38.
[28]Baxter GF.The natriuretic peptides.Basic Res Cardiol. 2004; 99(2):71-75.
[29]Tremblay J, Desjardins R, Hum D, et al.Biochemistry and physiology of the natriuretic peptide receptor guanylyl cyclases. Mol Cell Biochem. 2002;230(1-2):31-47.
[30]Firth JD, Raine AE, Ledingham JG.Raised venous pressure: a direct cause of renal sodium retention in oedema?Lancet. 1988;1(8593):1033-1035.
[31]Riter HG, Redfield MM, Burnett JC,et al.Nonhypotensive low-dose nesiritide has differential renal effects compared with standard-dose nesiritide in patients with acute decompensated heart failure and renal dysfunction.J Am Coll Cardiol. 2006;47(11):2334-2335.
[32]Elkayam U, Ng TM, Hatamizadeh P, et al.Renal Vasodilatory Action of Dopamine in Patients With Heart Failure: Magnitude of Effect and Site of Action.Circulation. 2008;117(2):200-205. |
| [1] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [2] | Nie Huijuan, Huang Zhichun. The role of Hedgehog signaling pathway in transforming growth factor beta1-induced myofibroblast transdifferentiation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 754-760. |
| [3] | Lang Limin, He Sheng, Jiang Zengyu, Hu Yiyi, Zhang Zhixing, Liang Minqian. Application progress of conductive composite materials in the field of tissue engineering treatment of myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3584-3590. |
| [4] | Sun Weixing, Zhao Yongchao, Zhao Ranzun. Mesenchymal stem cell transplantation in the treatment of myocardial infarction: problems, crux and new breakthrough [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3103-3109. |
| [5] | Chen Siyu, Li Yannan, Xie Liying, Liu Siqi, Fan Yurong, Fang Changxing, Zhang Xin, Quan Jiayu, Zuo Lin. Thermosensitive chitosan-collagen composite hydrogel loaded with basic fibroblast growth factor retards ventricular remodeling after myocardial infarction in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2472-2478. |
| [6] | Qiao Yuqi, Fu Rongchang, Zhang Lihong. Effects of sand therapy on hemodynamics in the femoral artery bifurcation at different degrees of stenosis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(8): 1218-1224. |
| [7] | Shang Qingqing, Zhou Jianye. Combination of hyaluronic acid hydrogel and bone marrow mesenchymal stem cells promotes cardiac function after myocardial infarction in rats (II) [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(34): 5559-5563. |
| [8] |
Chen Siyu, Zhang Tao, Yin Wenjuan, Cai Lei, Li Yannan, Xie Liying, Zuo Lin.
Changes of cardiac function in rats with myocardial
infarction after umbilical cord-derived mesenchymal stem cell transplantation:
a meta-analysis |
| [9] | Zhang Chaohui, Zhao Feng, Feng Yunpeng, Wang Wenbin, Kuang Baoping, Huang He. Research progress and medical application of modeling and simulation of cardiovascular system [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(7): 1115-1121. |
| [10] | Bao Mixia, Zhou Ping, Guo Feng, Wang Jia. Numerical simulation of bifurcating blood vessel flow under overload [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 551-555. |
| [11] | He Jigang, Xie Qiaoli, Wang Zihao, Yan Dan, Zhang Hongbo. Time-volume variation in miR-330-3p expression in GATA-4-overexpressing bone marrow-derived mesenchymal stem cell exosomes [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(29): 4617-4622. |
| [12] | Zhao Guangqiang. Tanreqing injection combined with ambroxol hydrochloride in treating heart failure and pulmonary infection caused by senile degenerative heart disease: a parallel, randomized, controlled clinical trial [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(27): 4402-4407. |
| [13] | Zhang Pin, Guo Ying, Gao Yajie, Wang Zhendong, Li Baiyi, Zhang Xiaomin, Niu Yuhu, Liu Zhizhen, Ma Lihui, Niu Bo, Guo Rui. Exosomes derived from human umbilical cord mesenchymal stem cells promote myocardial repair after myocardial infarction under hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(17): 2630-2636. |
| [14] | Chen Yili1, Lao Yonghua2, Zhang Shaoqun1, Wu Baofeng3, Li Yikai1 . Hydrodynamic model of carotid artery atherosclerosis: hemodynamic changes of carotid atherosclerotic plaques under cervical rotatory manipulation [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(15): 2403-2308. |
| [15] | Zhao Liang, Qiu Xiaona, Li Xiafei. Research progress of myocardial scaffolds in the treatment of myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(14): 2279-2284. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||